Site
Select your branch
Digital future: When will digital health dominate healthcare?
The promise of digital health
In the last decade, digital technologies changed almost every aspect of our lives; from how we work and learn to how we order food.
The only field where the digital revolution is slower than expected is healthcare.
The promise of a better healthcare system emerging from the digital era was made more than a decade ago, but there are still many obstacles to its meaningful implementation. Although a lot of pilot programs have been launched, the impact on routine healthcare practice has been limited so far.
We wanted to explore when and how digital health will become the driving force in healthcare.
What is digital health?
Before we dive into the fascinating world of digital health applications, however, let’s first try to understand a couple of key terms.
Is there a difference between digital medicine and digital health? What are digital treatments?
Even though these definitions are not set in stone and there are a lot of borderline cases, it is important to understand what the different terms mean.
Digital health includes all software-based technologies related to improving human wellness. These tools do not necessarily involve clinically relevant information but they use health-related data to improve people’s lifestyles as well as give operational support to healthcare professionals. No regulatory supervision is required since they are not classified as medical devices.
Digital medicine products go one level deeper; they can measure and/or intervene directly on people’s health with or without pharmacological or human assistance. They all require clinical evidence since their efficacy needs to be proven before commercialization. In case they are classified as medical devices and/or being involved in the development of other devices or drugs, the oversight of specific regulatory bodies becomes mandatory.
Digital therapeutics technologies have the primary goal to prevent, treat or manage a specific physical, psychological or behavioural condition. Every product needs clinical evidence and real-world data. Because of their therapeutic intervention, regulatory bodies need to approve product claims (e.g. in terms of efficacy, risks, treatment duration, use cases).
How niche technologies became mainstream?
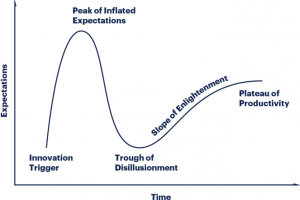
Let’s now look at digital health solutions from a technology adoption perspective, which has been described by the Gartner Hype Cycle for Emerging Technologies in 1995. As shown by the plot below, five main stages have been observed in most (but not all) technologies’ adoption journeys.
Where is digital health on the expectations and time axes? Usually, the “only” (or at least the most important) challenge is technology readiness, but since healthcare is a very complex system, there are different challenges to be overcome, such as regulatory approval, users’ adoption model and government policies. The most advanced among the digital health solutions are telehealth, online triaging or remote monitoring and connected devices which have reached the plateau of productivity. Home health monitoring is thought to have passed the trough of disillusionment in 2009 and 2012, while secure chats (patient to doctor), remote testing, machine learning, and AI symptoms checker is now believed to be at the slope of enlightenment stage. Mobile health monitoring passed the peak of inflated expectations in 2013 and the trough of disillusionment in 2014 and is now reaching the plateau of productivity.
All of the digital health solutions which have reached the productivity plateau, have overcome not only the technological challenges, but also achieved clinical validation and hence could demonstrate evidence-based benefit to patients.
On the other hand, digital technologies that are on the path of enlightenment phase are still lacking some core triggers; for example, secure chats have no unambiguous architecture to secure data privacy and oversight while AI symptoms checkers are still lacking large scale clinical validation, which is key to increasing adoption from pilot programmes.
Regarding the home and mobile health monitoring applications, they are definitely closer to becoming mainstream than all the others. What they are still missing is finding out a method to unlock the growth and scaling up trigger, which is arguably the last step nobody has solved yet.
As it always happens in innovation, being the pioneer is one of the hardest possible roles, since you need to navigate the unknown at your own risk. Once a few pioneers will crack the puzzle, many are going to follow and the revolution will finally arrive.
How to drive digital health forward?
Healthcare is a large and complex ecosystem, difficult to penetrate for external innovators and as there are many interests at stake, stakeholder alignment is one of the biggest challenges. A key issue often experienced by digital health startups is gaining access to healthcare providers to first prove the effectiveness of the given digital solution and then to scale up sales. Procurement processes are often very complex and budgets are tight. It is undeniably hard to navigate the entire ecosystem and with so many new digital solutions being created each day, most people, especially clinicians and patients, are unsure about what to expect from this wave of innovation. In order to drive adoption of the best solutions, it is essential to standardise the evaluation of the different digital tools.
Digital health companies are also trying to create their own unique operational model. It is becoming increasingly evident that the modus operandi of traditional Software as a Service (SaaS) companies: “move fast and break things” might not be well suited for healthcare start-ups, which need to appeal to patients/users but also doctors and regulators for whom safety and efficacy are key objectives. Therefore multi-stakeholder engagement including patients, doctors and regulators while developing a new product becomes paramount.
Dialog seems indeed to be the key.
Digital health is a very broad field, which merges several disciplines and professions. While multidisciplinary settings always provide opportunities for exchanging different ideas and perspectives on the same topic, there are also some fundamental challenges such as the difficulty to find a common language to efficiently work together. That is because the different stakeholders who need to interact have their own sets of definitions and operational frameworks. Nevertheless, when passionate people are brought together, progress can be achieved. A big role in driving this positive change is also with third sector organisations and notable examples of groups involved in creating dialog are the Digital Medicine (DiMe) Society, the Digital Therapeutics Alliance, Node.Health or the HealthXL.
The role of national governments
Whether a country has a public or private healthcare system, the role of the government is without any doubt of critical importance.
Starting from the “classical” prescription drugs model, a lot can be done to favour the adoption of digital health solutions to the benefit of patients first, then also the overall economy.
For example, Denmark has already developed an infrastructure to securely store health data, which is protected by the government; while Estonia has invested in blockchain technology to secure the centralized health data the country has collected over the last several years and will continue to do so.
The UK and Germany are other well-known examples. The former successfully trialled a telehealth system in 2017, while the latter has recently given doctors permission to prescribe health apps as part of a treatment regime to all insured patients, starting in 2020.
Another example of a positive effort to implement digital health has been made by Sweden, which provides adults with access to their health-related data, including illness and treatments, in addition to allowing them to send secure messages to hospitals. This is definitely a strong example of how everyone can be empowered, informed and educated about their health and everything suggests it will become even more critical when data from genome-based personalized medicine becomes available.